Nr 509 cough soap note - Study guides, Class notes & Summaries
Looking for the best study guides, study notes and summaries about Nr 509 cough soap note? On this page you'll find 31 study documents about Nr 509 cough soap note.
All 31 results
Sort by

-
NR 509 Week 3 class discussion, Complete Solution
- Exam (elaborations) • 91 pages • 2023
-
- $12.48
- + learn more
NR 509 Week 3 class discussion, Complete Solution Week 3: Neurologic, Musculoskeletal, and Cardiopulmonary Assessment 11 unread reply.6464 replies. Using a friend, family member, or colleague, perform a neurovascular (include all cranial nerves), musculoskeletal, and cardiopulmonary (includes the heart, lungs, and peripheral vasculature) exam. Document the physical examination findings in the SOAP note format. Even though your patient may have abnormal findings, you must document the expected...
-
NR 509 Week 6 SOAP NOTE.
- Exam (elaborations) • 20 pages • 2022
-
- $10.49
- + learn more
NR 509 Week 6 SOAP NOTE. History of Present Illness (HPI) Chief Complaint (CC) “I have been coughing a lot” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset Started 5 days ago Location Throat an...

-
NR 509 WEEK 2 SOAP Note Template
- Summary • 18 pages • 2023
-
- $9.99
- + learn more
NR 509 WEEK 2 SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Ratingwh 0/10 Allergies (and reaction) 170 cm 89 kg 140/ 81 89 20 98.5 97 Medica tion: Penicillin – rash/hives Food: n/a Environment: Cats – Sneezing, itching, asthma attacks, rhinorrhea History of Present Illness (HPI) Chief Complaint (CC) breathing problems, chest tightness, and wheezing CC is a BRIEF statement identifying why the patient is here - in the patie...

-
NR 509 WEEK 5 SOAP Note ABDOMINAL TEMPLATE
- Class notes • 14 pages • 2024
- Available in package deal
-
- $10.49
- + learn more
NR 509 WEEK 5 SOAP Note ABDOMINALTemplate Initials: EP Age: 78 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 157.4 120 lbs 110/ .0 C 99% 6/10 Medication: KNDA Foo d: No food allergies Environment: Latex “itchy skin rash” History of Present Illness (HPI) Chief Complaint (CC) “I have some pain in my belly. . . and I'm having difficulty going to the bathroom.” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headac...

-
NR 509 WEEK 6 SOAP Note Template
- Summary • 17 pages • 2023
-
- $9.99
- + learn more
NR 509 WEEK 6 SOAP Note Template Initials: D.R. Age: 8 years old Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 127 cm 40.9 kg 120/ 76 100 28 37.2 C 96% Medication: No known drug allergies Food: No known food allergies Environment: No known environmental allergies History of Present Illness (HPI) Chief Complaint (CC) “I have been coughing a lot” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "he...

-
NR 661 WEEK 6 APN CAPSTONE PORTFOLIO PART 2 RATED A+
- Exam (elaborations) • 57 pages • 2023
-
- $14.99
- + learn more
Running head: APN CAPSTONE PORTFOLIO PART 2 1 NR 661 WEEK 6 APN CAPSTONE PORTFOLIO PART 2 APN Capstone Part 2.1: Synthesis of Knowledge Table of Contents APN Capstone Portfolio Part 2 3 Exemplar # 1 NUR 507 Pathophysiology March 2017 3 Identify and Explain 4 Connect 5 Reflection 5 Exemplar # 2 Nr503 Evaluation Of Epidemiological Problem Paper, 2017 6 Identify and Explain 10 Connect 11 Reflection 12 Exemplar # 3 NR512: Fundamentals of Nursing Informatics May 2017 12 Identi...

-
NR 509 WEEK 5 SOAP Note Template
- Summary • 16 pages • 2023
-
- $9.99
- + learn more
NR 509 WEEK 5 SOAP Note Template Initials: E.P. Age: 78 years old Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 62 inches 54.43 kg 110/ 70 92 16 37.0 C 99% Medication: No known drug allergies Food: No known food allergies Environment: Reports latex allergy-contact dermatitis History of Present Illness (HPI) Chief Complaint (CC) “Pain in my belly” and “I’m having difficulty going to the bathroom” CC is a BRIEF statement identifying why the patie...
-
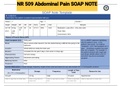
Exam (elaborations) NR 509 Abdominal Pain SOAP NOTE
- Exam (elaborations) • 12 pages • 2022
-
- $5.49
- 1x sold
- + learn more
Exam (elaborations) NR 509 Abdominal Pain SOAP NOTE t Weight BP HR RR Temp SPO2 Pain Allergies 157.48 (5’2”) 54 kg (120 lbs) 110/ 70 92 16 37.0 C 99% 6/10 Medication: Latex (Rxn - itchy skin rash) Food: NKA Environment: NKA History of Present Illness (HPI) Chief Complaint (CC) “Belly pain” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient h...
-
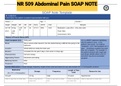
NR 509 Abdominal Pain SOAP NOTE (NR509)
- Exam (elaborations) • 12 pages • 2021
-
- $9.99
- + learn more
Exam (elaborations) NR 509 Abdominal Pain SOAP NOTE (NR509) SOAP Note Template Initials: E.P. Age: 78 Gender: F Height Weight BP HR RR Temp SPO2 Pain Allergies 157.48 (5’2”) 54 kg (120 lbs) 110/ 70 92 16 37.0 C 99% 6/10 Medication: Latex (Rxn - itchy skin rash) Food: NKA Environment: NKA History of Present Illness (HPI) Chief Complaint (CC) “Belly pain” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache...

-
NR 509 Week 5 Soap Note (NR509)
- Exam (elaborations) • 11 pages • 2021
-
- $8.99
- + learn more
Exam (elaborations) NR 509 Week 5 Soap Note (NR509) SOAP NOTES TEMPLATE S: Subjective Information the patient or patient representative told you. Initials: EP Age: 78 Gender: Female Height: 5’2” Weight: 120 lbs BP: 110/70 HR:92 Temp: 37.0 C SPO2: 99 RR: 16 Pain (1-10): 6 Allergies: Medication: NKDA Food: none Environment: Latex—“itchy rash” History of Present Illness (HPI) Chief Complaint (CC): “pain in my belly” and difficulty going to the bathroom Onset: Con...

How much did you already spend on Stuvia? Imagine there are plenty more of you out there paying for study notes, but this time YOU are the seller. Ka-ching! Discover all about earning on Stuvia


