Exambank12
On this page, you find all documents, package deals, and flashcards offered by seller EXAMBANK12.
- 489
- 0
- 0
Community
- Followers
- Following
9 Reviews received
489 items
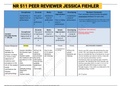
Exam (elaborations) NR 511 PEER REVIEWER JESSICA FIEHLER
Exam (elaborations) NR 511 PEER REVIEWER JESSICA FIEHLER R 511 PEER REVIEWER JESSICA FIEHLER NR511 Peer Review Template and 4) Identifies the typical clinical presentation seen in a patient with the disease (4 critical elements). the typical clinical presentation seen in a patient with the disease. Jessica presented eight (4 critical elements must be noted) different typical ways AOE could present in the clinical setting. Publication & Applicability in Primary Care ...
- Exam (elaborations)
- • 5 pages •
Exam (elaborations) NR 511 PEER REVIEWER JESSICA FIEHLER R 511 PEER REVIEWER JESSICA FIEHLER NR511 Peer Review Template and 4) Identifies the typical clinical presentation seen in a patient with the disease (4 critical elements). the typical clinical presentation seen in a patient with the disease. Jessica presented eight (4 critical elements must be noted) different typical ways AOE could present in the clinical setting. Publication & Applicability in Primary Care ...
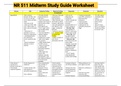
Exam (elaborations) NR 511 Midterm Study Guide Worksheet
Exam (elaborations) NR 511 Midterm Study Guide Worksheet ase Risk Subjective Finding Objective Findings Diagnostics Treatment Education GI DISORDERS Appendicitis -Most common between 10-30yrs; but can occur at any age; rare in infants and older adults -men more at risk - Diets low in fiber, high in fat, refined sugars, & other carbs at increased risk. - Obstruction of appendix is cause of majority of appendicitis - contributing factors: Intra-abdominal tumors, positi...
- Exam (elaborations)
- • 111 pages •
Exam (elaborations) NR 511 Midterm Study Guide Worksheet ase Risk Subjective Finding Objective Findings Diagnostics Treatment Education GI DISORDERS Appendicitis -Most common between 10-30yrs; but can occur at any age; rare in infants and older adults -men more at risk - Diets low in fiber, high in fat, refined sugars, & other carbs at increased risk. - Obstruction of appendix is cause of majority of appendicitis - contributing factors: Intra-abdominal tumors, positi...

Exam (elaborations) NR 511 DISCUSSION PART 1 WEEK 3 (PERTINENT INFORMATION)
Exam (elaborations) NR 511 DISCUSSION PART 1 WEEK 3 (PERTINENT INFORMATION) A 19-year-old male freshman college student presents to the student health center today with complaints of bilateral eye discomfort. Upon further questioning you discover the following subjective information regarding the chief complaint. History of Present Illness Onset 2-3 days ago Location Both eyes Duration Constant Characteristics Both eyes feel "gritty" with mild to moderate amount of discomfort. Furth...
- Exam (elaborations)
- • 6 pages •
Exam (elaborations) NR 511 DISCUSSION PART 1 WEEK 3 (PERTINENT INFORMATION) A 19-year-old male freshman college student presents to the student health center today with complaints of bilateral eye discomfort. Upon further questioning you discover the following subjective information regarding the chief complaint. History of Present Illness Onset 2-3 days ago Location Both eyes Duration Constant Characteristics Both eyes feel "gritty" with mild to moderate amount of discomfort. Furth...

Exam (elaborations) NR 509 WEEK 8 QUIZ ASSESSMENT
Exam (elaborations) NR 509 WEEK 8 QUIZ ASSESSMENT Quiz #8 Question 1 2 / 2 pts It is important to approach each clinical experience with an open mind and positive attitude? Correct! True False NP students should keep an open mind and positive attitude throughout the clinical rotation. The clinical site might not be you preferred environment; but you can still make the most out of the experience. Question 2 2 / 2 pts If I arrive at my clinical site and my preceptor who was appro...
- Exam (elaborations)
- • 3 pages •
Exam (elaborations) NR 509 WEEK 8 QUIZ ASSESSMENT Quiz #8 Question 1 2 / 2 pts It is important to approach each clinical experience with an open mind and positive attitude? Correct! True False NP students should keep an open mind and positive attitude throughout the clinical rotation. The clinical site might not be you preferred environment; but you can still make the most out of the experience. Question 2 2 / 2 pts If I arrive at my clinical site and my preceptor who was appro...

Exam (elaborations) NR 509 Week 5 Soap Note
Exam (elaborations) NR 509 Week 5 Soap Note Initials: EP Age: 78 Gender: Female Height: 5’2” Weight: 120 lbs BP: 110/70 HR:92 Temp: 37.0 C SPO2: 99 RR: 16 Pain (1-10): 6 Allergies: Medication: NKDA Food: none Environment: Latex—“itchy rash” History of Present Illness (HPI) Chief Complaint (CC): “pain in my belly” and difficulty going to the bathroom Onset: Constipation 5 days ago with the exception of an episode of was watery diarrhea 3 days ago Location: “l...
- Exam (elaborations)
- • 11 pages •
Exam (elaborations) NR 509 Week 5 Soap Note Initials: EP Age: 78 Gender: Female Height: 5’2” Weight: 120 lbs BP: 110/70 HR:92 Temp: 37.0 C SPO2: 99 RR: 16 Pain (1-10): 6 Allergies: Medication: NKDA Food: none Environment: Latex—“itchy rash” History of Present Illness (HPI) Chief Complaint (CC): “pain in my belly” and difficulty going to the bathroom Onset: Constipation 5 days ago with the exception of an episode of was watery diarrhea 3 days ago Location: “l...
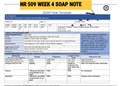
Exam (elaborations) NR 509 WEEK 4 SOAP NOTE
Exam (elaborations) NR 509 WEEK 4 SOAP NOTE nitials: BF Age: 58 Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 5’ 11 197lbs 146/ 90 104 19 36.7C 98% Medication: Codeine : reports causes nausea and vomiting Food: none Environment: none History of Present Illness (HPI) Chief Complaint (CC) Chest pain CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a...
- Exam (elaborations)
- • 8 pages •
Exam (elaborations) NR 509 WEEK 4 SOAP NOTE nitials: BF Age: 58 Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 5’ 11 197lbs 146/ 90 104 19 36.7C 98% Medication: Codeine : reports causes nausea and vomiting Food: none Environment: none History of Present Illness (HPI) Chief Complaint (CC) Chest pain CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a...

Exam (elaborations) NR 509 Week 1 Study Guide
Exam (elaborations) NR 509 Week 1 Study Guide 1. After completing an initial assessment of a patient, the nurse has charted that his respirations are eupneic and his pulse is 58 beats per minute. These types of data would be. A. Objective B. Reflective C. Subjective D. Introspective 2. A patient tells the nurse that he is very nervous, is nauseated and feels hot. These types of data would be A. Objective B. Reflective C. Subjective D. Introspective 3. The patients record, labor...
- Exam (elaborations)
- • 22 pages •
Exam (elaborations) NR 509 Week 1 Study Guide 1. After completing an initial assessment of a patient, the nurse has charted that his respirations are eupneic and his pulse is 58 beats per minute. These types of data would be. A. Objective B. Reflective C. Subjective D. Introspective 2. A patient tells the nurse that he is very nervous, is nauseated and feels hot. These types of data would be A. Objective B. Reflective C. Subjective D. Introspective 3. The patients record, labor...

Exam (elaborations) NR 509 Shadow Health Focused Exam Abdominal Education Empathy
Exam (elaborations) NR 509 Shadow Health Focused Exam Abdominal Education Empathy During the patient interview, there are a number of opportunities to provide patient education and empathy. The opportunities listed below are those identified by nursing experts to be of particular importance to this patient. A Model Statement is provided as an example of an appropriate response to each opportunity. Opportunities marked as Not Encountered are opportunities that were not elicited in th...
- Exam (elaborations)
- • 33 pages •
Exam (elaborations) NR 509 Shadow Health Focused Exam Abdominal Education Empathy During the patient interview, there are a number of opportunities to provide patient education and empathy. The opportunities listed below are those identified by nursing experts to be of particular importance to this patient. A Model Statement is provided as an example of an appropriate response to each opportunity. Opportunities marked as Not Encountered are opportunities that were not elicited in th...

Exam (elaborations) NR 509 SHADOW HEALTH Abdominal Pain Physical Assessment Assignment Results Completed
Exam (elaborations) NR 509 SHADOW HEALTH Abdominal Pain Physical Assessment Assignment Results Completed ocumentation / Electronic Health Record This study source was downloaded by from CourseH on 07-26-2021 12:26:30 GMT -05:00 This study resource was shared via CourseH 12/10/2018 Abdominal Pain Physical Assessment Assignment | Completed | Shadow Health Student Documentation Model Documentation Respiratory: Patient denies any coughing or sore throat. Denies any difficulty breathing o...
- Exam (elaborations)
- • 4 pages •
Exam (elaborations) NR 509 SHADOW HEALTH Abdominal Pain Physical Assessment Assignment Results Completed ocumentation / Electronic Health Record This study source was downloaded by from CourseH on 07-26-2021 12:26:30 GMT -05:00 This study resource was shared via CourseH 12/10/2018 Abdominal Pain Physical Assessment Assignment | Completed | Shadow Health Student Documentation Model Documentation Respiratory: Patient denies any coughing or sore throat. Denies any difficulty breathing o...

Exam (elaborations) NR 509 Quiz 7
Exam (elaborations) NR 509 Quiz 7 During an examination of an aging male the FNP recognizes that normal changes to expect would be: Decrease in penis size 2) During a health history, a 22-year-old woman asks “can I get that vaccine for HPV? I have gentle warts and I’d like them to go away!” What is the FNP‘s best response? Vaccine cannot protect you if you already have an HPV infection 3) During a speculum inspection of the vagina the FNP would expect to see what at the end of...
- Exam (elaborations)
- • 3 pages •
Exam (elaborations) NR 509 Quiz 7 During an examination of an aging male the FNP recognizes that normal changes to expect would be: Decrease in penis size 2) During a health history, a 22-year-old woman asks “can I get that vaccine for HPV? I have gentle warts and I’d like them to go away!” What is the FNP‘s best response? Vaccine cannot protect you if you already have an HPV infection 3) During a speculum inspection of the vagina the FNP would expect to see what at the end of...

Exam (elaborations) Pharmacology 2017 Hesi PN Specialty V2-
Exam (elaborations) Pharmacology 2017 Hesi PN Specialty V2-
Exam (elaborations) TEST BANK NCLEX Saunders Comprehensive Review for NCLEX-PN, ISBN: 9780721677941
Exam (elaborations) FNP NR 506 LEIK EXAM TIPS TEST PREP
Exam (elaborations) NURSING 465 MED-SURG TEST FINAL EXAM TEST BANK